Cataracts are a common eye condition that can have a significant impact on a person’s vision. With advancements in medical technology, there are now several different types of cataracts surgery techniques available. Understanding these techniques can help individuals make informed decisions about their treatment options and achieve the best possible outcomes for their vision.
Defining Cataract and Its Impact on Vision
Cataract refers to the clouding of the natural lens of the eye, which is responsible for focusing light onto the retina. As a result, individuals with cataracts may experience blurry vision, difficulty seeing in low light, and increased sensitivity to glare. Cataracts can develop due to age, injury, certain medications, or underlying medical conditions such as diabetes. If left untreated, cataracts can significantly impair a person’s ability to perform daily tasks and lead to a diminished quality of life.
The Anatomy of the Eye and Cataract Formation
The eye is a complex organ composed of various structures, including the cornea, iris, lens, and retina. The cornea is the clear, dome-shaped front surface of the eye that helps to focus incoming light. Behind the cornea is the iris, which is the colored part of the eye that controls the size of the pupil. The pupil is the black center of the eye that allows light to enter. Located behind the iris is the lens, a transparent structure that plays a crucial role in focusing light onto the retina. The retina, located at the back of the eye, is responsible for converting light into electrical signals that are sent to the brain, allowing us to see.
Over time, the proteins in the lens can clump together and form cataracts, leading to the aforementioned vision problems. This clumping of proteins can occur due to a variety of factors, including age-related changes in the lens, exposure to ultraviolet radiation from the sun, smoking, and certain medical conditions such as diabetes. As the proteins clump together, they create a cloudy area in the lens, which obstructs the passage of light and impairs vision.
The Symptoms and Diagnosis of Cataracts
Common symptoms of cataracts include blurred vision, difficulty seeing at night, sensitivity to light, and the perception of halos around lights. These symptoms can vary in severity and may worsen over time. If you are experiencing any of these symptoms, it is important to visit an eye care professional who can perform a comprehensive eye exam to diagnose cataracts.
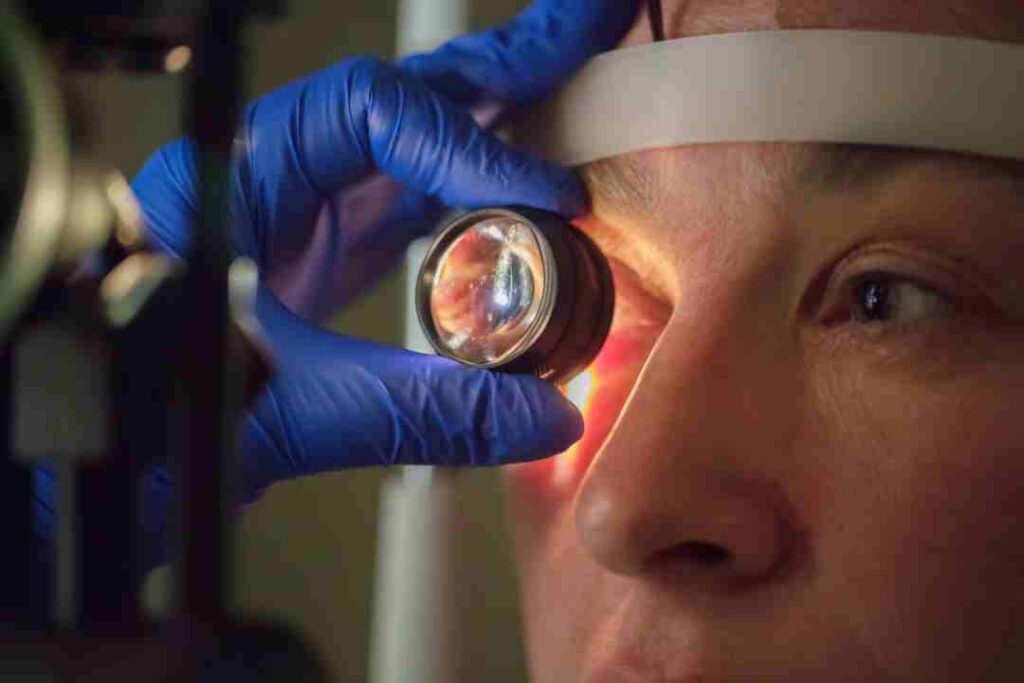
During the eye exam, the eye care professional will evaluate your visual acuity, which measures how well you can see at various distances. They may also perform a slit-lamp examination, which involves using a specialized microscope to examine the structures of the eye, including the lens. Additionally, they may dilate your pupils using eye drops to get a better view of the lens and the back of the eye. This allows them to assess the severity of the cataract and determine the most appropriate treatment options.
It is important to note that cataracts can develop in one or both eyes, and they can progress at different rates. Therefore, it is essential to monitor your vision regularly and seek prompt medical attention if you notice any changes or symptoms suggestive of cataracts.
An Overview of Cataract Surgery
Cataract surgery is a common and highly successful procedure aimed at removing the clouded lens and replacing it with an artificial intraocular lens (IOL). The primary goals of cataract surgery are to improve vision, minimize dependence on glasses or contact lenses, and enhance overall quality of life.
Cataracts, which are the leading cause of vision loss in adults over the age of 40, occur when the natural lens of the eye becomes cloudy. This cloudiness can cause blurred vision, difficulty seeing in low light conditions, and increased sensitivity to glare. Cataract surgery is the only effective treatment for cataracts and can significantly improve a person’s visual acuity and quality of life.
The Purpose and Goals of Cataract Surgery
A cataract surgery aims to remove the clouded lens that is obstructing light from properly reaching the retina. By replacing the natural lens with an artificial IOL, the surgeon can restore clear vision and address other visual abnormalities, such as astigmatism, if necessary.
The surgery itself is typically performed on an outpatient basis and is relatively quick, usually taking less than 30 minutes to complete. The procedure involves making a small incision in the eye, breaking up the clouded lens using ultrasound waves or laser technology, and removing the fragments. Once the lens is removed, the artificial IOL is inserted into the eye, where it will permanently remain.
After the surgery, patients may experience some mild discomfort, redness, and blurred vision, but these symptoms usually subside within a few days. It is important to follow the postoperative instructions provided by the surgeon, which may include using prescribed eye drops, avoiding strenuous activities, and wearing an eye shield at night to protect the eye during sleep.
Preparing for Cataract Surgery: What to Expect
In preparation for cataract surgery, your eye care professional will conduct a thorough evaluation of your eye health and discuss any preoperative instructions. This may involve avoiding certain medications, fasting before the procedure, and arranging for transportation on the day of surgery. Additionally, your surgeon will discuss the different types of cataract surgery techniques available and help you choose the most appropriate one for your individual needs and preferences.
During the evaluation, your eye care professional will measure the shape and size of your eye, assess your visual acuity, and check for any other eye conditions that may affect the outcome of the surgery. They may also perform additional tests, such as an ultrasound or optical coherence tomography (OCT), to obtain detailed images of your eye’s structures.
Once the evaluation is complete and the surgery is scheduled, it is important to follow any preoperative instructions provided by your eye care professional. This may include avoiding certain medications, such as blood thinners, that can increase the risk of bleeding during surgery. Fasting before the procedure is also typically required to ensure that your stomach is empty, reducing the risk of complications related to anesthesia. You can also read about Opening a Sydney Eye Clinic in a Community Health Centre by visiting https://bockhealingcenter.com/opening-a-sydney-eye-clinic-in-a-community-health-centre/
On the day of surgery, it is important to have someone accompany you to the surgical center or hospital, as you will not be able to drive yourself home afterwards. The surgery itself is usually performed under local anesthesia, meaning that you will be awake but your eye will be numbed to prevent any pain or discomfort. Some patients may also be given a sedative to help them relax during the procedure.
In conclusion, cataract surgery is a highly effective procedure that can significantly improve vision and quality of life for individuals with cataracts. By removing the clouded lens and replacing it with an artificial IOL, cataract surgery restores clear vision and reduces the need for glasses or contact lenses. Preparing for cataract surgery involves a thorough evaluation of eye health, discussion of preoperative instructions, and choosing the most appropriate surgical technique. Following the surgery, it is important to adhere to the postoperative instructions provided by the surgeon to ensure proper healing and optimal visual outcomes.
Exploring the Different Techniques of Cataract Surgery
There are several different techniques used in cataract surgery, each with its own advantages and considerations. The two most commonly utilized techniques include phacoemulsification and extracapsular cataract surgery.
Phacoemulsification: The Most Common Technique
Phacoemulsification involves using ultrasonic energy to break up the cloudy lens into small fragments, which are then suctioned out through a small incision. This technique is highly precise and minimizes trauma to the surrounding tissues, resulting in a faster recovery and reduced risk of complications.
Extracapsular Cataract Surgery: When is it Used?
Extracapsular cataract surgery is typically reserved for more advanced cataracts or cases where phacoemulsification may not be feasible. In this technique, the surgeon removes the cloudy lens in one piece through a larger incision. While this approach may require a longer recovery period, it can be beneficial in certain situations where phacoemulsification may not be suitable.
Intracapsular Cataract Surgery: The Traditional Approach
Intracapsular cataract surgery is a less commonly performed technique where the entire lens, including the capsule that surrounds it, is removed. This approach is now rarely used due to the availability of more advanced and less invasive techniques like phacoemulsification.
Comparing the Techniques: Pros and Cons
When considering the different cataract surgery techniques, various factors come into play. These include the severity of the cataract, the patient’s overall eye health, and any unique considerations or preferences. It is essential to discuss these aspects with your surgeon to determine the most suitable technique for your specific needs.
Factors Influencing the Choice of Technique
The choice of cataract surgery technique may be influenced by factors such as the density and location of the cataract, the surgeon’s expertise and experience, the patient’s medical history, and the presence of other eye conditions or complications. Working closely with your surgeon will ensure that the most appropriate technique is selected to optimize your surgical outcome.
Risks and Complications Associated with Each Technique
While cataract surgery is generally safe and effective, it is essential to be aware of the potential risks and complications associated with each technique. These may include infection, bleeding, inflammation, postoperative inflammation, and changes in intraocular pressure. Your surgeon will discuss these risks in detail and provide guidance on how to minimize them.
Post-Surgery Care and Recovery
Successful cataract surgery also depends on proper postoperative care and adherence to the surgeon’s instructions. This includes both immediate post-surgery care and long-term recovery and vision improvement strategies.
Immediate Post-Surgery Care
Following cataract surgery, your surgeon will provide specific instructions on how to care for your eyes. This may involve using prescribed eye drops, wearing a protective shield during sleep, and avoiding activities that put pressure on the eyes, such as heavy lifting or strenuous exercises. Regular follow-up appointments will be scheduled to monitor your progress and ensure that your eyes are healing properly.
Long-Term Recovery and Vision Improvement
Although vision improvement is often noticeable soon after cataract surgery, complete healing may take some time. It is essential to be patient and follow your surgeon’s guidance for optimal recovery. Over the following weeks, your vision will continue to improve, and you may be advised to use protective eyewear and gradually resume normal activities. It is also essential to attend regular eye exams to monitor your vision and address any concerns that may arise.
Understanding the different types of cataract surgery techniques is crucial for individuals who are considering or preparing for cataract surgery. By being well-informed, patients can have productive discussions with their surgeons, make informed decisions about their treatment options, and ultimately achieve the best possible outcomes for their vision. Remember, your eye health is essential, and seeking professional advice is the first step towards clearer vision and improved quality of life.