Although widespread rapid antigen test screening campaigns among the general public may seem to be a viable tactic for directing containment efforts, the challenges involved with such a plan should not be underestimated, and their effectiveness is still in question.
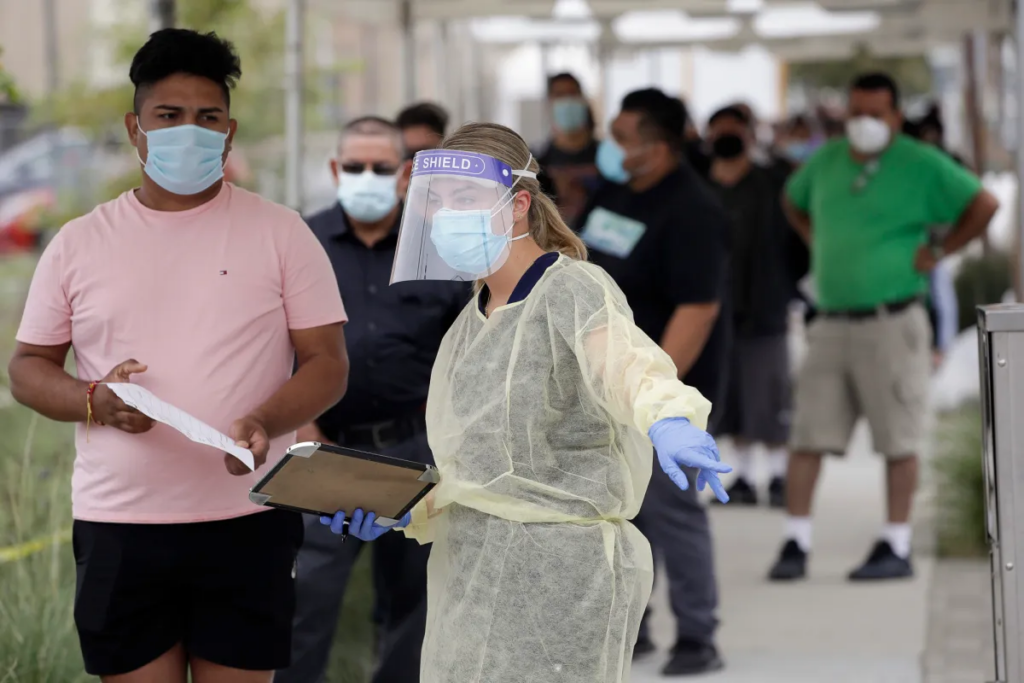
Testing millions of people each week, along with all of the required pre-and post-analytical work, is, first and foremost, a time-consuming and labor-intensive operation. Once again, in terms of capacity and expense for testing on a big scale, such as millions of people, rapid antigen tests are now the only practical option. However, as was said above, there are issues because of their current poor performance. The problem of low prevalence in the general population and, thus, the high frequency of false positives, will continue to be a worry even if the performance of rapid antigen test improves over time.
In other words, a significant portion (perhaps more than 50%) of all “positive” fast antigen testing will really be false positives. It may be difficult for people to accept fast antigen testing if those who get a positive test result are expected to isolate themselves, which would be necessary for the approach to be effective.
Large-scale management of this is challenging
Because of this, even if they did not have the virus in their system, many people would still have limits in their day-to-day activities, including their ability to work. If such a scenario is plausible, officials must determine if there is sufficient public support for it to be effectively implemented.
Mass screening can only be effective if people are willing to get tested and if those who test positive quickly segregate. If people are hesitant to isolate because they question the validity of the test results, this is especially true if they think the results are false,
Population-wide screening is now being tested in a number of countries, but the programs are complicated and costly to carry out, and the results have been uneven so far. Depending on the conditions, next-generation sequencing (NGS) may, in the future, be a viable choice from a technological standpoint.
However, the technology behind these rapid antigen tests is still in its infancy. NGS is a very sensitive and focused test modality that can yield very high throughput rates at incredibly cheap costs. Next-generation sequencing (NGS), which can test up to 10,000 samples at a time with a turnaround time of 24 to 48 hours for results, is being used by certain businesses and laboratories to increase COVID-19 testing capacity.
If the COVID-19 quick antigen test findings are negative, what should I do?
In less than an hour, SARS-CoV-2 antigens may be found in nasopharyngeal swab samples using the COVID-19 rapid antigen tests, which are membrane-based lateral flow immunoassays. A COVID-19 fast antigen test may be used to detect the presence of SARS-CoV-2 viral antigens in human bodies, which can then be used to start preventative isolation procedures to stop the virus’s spread. One of these rapid antigen tests may detect someone who is at or close to the peak of an illness. The question then becomes: How should I interpret the antigen rapid test results? Visit http://bockhealingcenter.com/making-the-most-of-your-rapid-antigen-tests/ to read about Making the most of your rapid antigen tests.
The COVID-19 fast antigen test’s structure Cassette
Two lines of antigen are coated on the COVID-19 antigen test cassette (the control line and the test line). If the sample has SARS-CoV-2 antigens, a colored line will emerge on the test strip, indicating that the sample has SARS-CoV-2 antibodies coated on the (T) Test line region and that the sample has SARS-CoV-2 antigens.
The lack of a colored line in the (T) Test line region indicates a negative result, proving that the antigens were not present in the sample. A colorful line in the (C) Control line section, which indicates that the test method was successfully applied and that the test components performed as expected, is always visible.
The valid rapid antigen tests results
A successful test leads to the appearance of two vibrant lines.
There must always be a colored line in the Control (C) section and another line in the Test (T) section (T). The sample included SARS-CoV-2 antigens, which led to a good outcome.
When the instructions are well followed, a positive antigen test result is thought to be reliable; however, when the instructions are not carefully followed, there is an increased risk of false-negative findings, meaning it is possible to have the virus while having a negative result. You can also read about the Outcome of the evaluation of rapid diagnostic assays for specific SARS-CoV-2 antigens (lateral flow devices) by clicking here.

In the Control (C) zone, a colored line appears when the outcome is negative.
There is no visible line in the Test (T) section
A colored line must always be visible in the Control (C) zone for the test to be considered valid, exactly as it is in the event of a good outcome. A negative result means that in this specific instance, the detection threshold for SARS-CoV-2 antigens in the sample has not been reached. There is still a chance of infection developing in the sample even if the sample contains too few antigens for the quick antigen assays to detect them.
If there is no control line, do not utilize these findings
Generally speaking, the most common reasons for the removal of the control line in the sample are inadequate diluent volume or improper procedural steps. Review the procedure, and if required, do the test using a different instrument.
Most rapid antigen tests may be completed at the patient’s bedside, and they are often inexpensive. The bulk of the rapid antigen tests that are currently allowed provides results in 15 minutes or less. Rapid antigen tests for SARS-CoV-2 are often less sensitive than real-time reverse transcription polymerase chain reaction (RT-PCR) and other nucleic acid amplification rapid antigen tests when it comes to detecting the presence of viral nucleic acid (NAATs). The presence of viral nucleic acid does not always indicate contagiousness, as shown by the fact that RT-PCR may identify small quantities of viral nucleic acid that cannot be grown.
Within 15 to 30 minutes after obtaining the findings of the rapid antigen tests, please make a choice. The outcome won’t be accurate if you recheck after a few hours.
