Rapid antigen tests may now be purchased over-the-counter in many nations, therefore it’s critical that we understand how to apply them. If a person has symptoms before a social event, rapid antigen tests might be very beneficial. The test results will be sent in around 15 minutes, which is substantially faster than traditional PCR testing. The test findings’ correctness, nevertheless, heavily depends on us.
Do we carefully abide by the instructions? Do we hand-wash before taking the test? Do we successfully gather the samples? Here’s how to get the most out of the Lepu SARS-CoV-2 Rapid Antigen Tests (self-test) and improve the likelihood that the results will be significant.

- Avoid eating or smoking when handling samples.
- Be mindful of the temperature and humidity in the laboratory: the reaction temperature should be between 15 and 30 degrees Celsius, and the humidity level should be under 70%.
- Prior to testing, wash your hands or put on clean gloves.
- Before testing, inspect the packaging. If the box is damaged or the product has passed its validity date, discard it.
- Perform rapid antigen tests one hour after removing the card from the foil bag.
- Comply with the directions in the user guide.
- Before testing, remove the double-sided sticky covering to avoid liquid splashing.
- Ensure that the dilution buffer is inserted into the appropriate well.
- To prevent moving the test card during testing, it should be put on a horizontal table. 10. Never mix or swap out different specimens.
- To prevent contamination, do not contact the swab’s head while opening the bag.
- Don’t gather specimens using already sterilized swabs.
- Patients who suffer from severe allergic rhinitis might have falsely positive test findings.
- Don’t put the goods in the refrigerator 15. Watch out for faulty test results Regardless of the outcome shown on the Test Line (T), if a purple-red band does not emerge in the Control Line (C), either the operating procedure is flawed, or the test kit is faulty. In this situation, retest precisely according to the instructions with a fresh test kit. Please let your local provider know if the issue reappears.
The Tests’ Use
Making sure the diagnostic kits are utilized properly is one of the biggest difficulties in providing them to everyone. Despite the fact that the rapid antigen test kits I just got from my state were quite easy to use, there are still several significant ways they might be misconstrued.
In order to use the kit, I was given, I had to swab both of my nostrils and then dip the swab into a liquid medium. I removed the swab and threw it away after swirling it around in the liquid. The liquid was then applied in three drops on a rectangular diagnostic test strip, and I watched as it wicked over the strip. After waiting the whole fifteen minutes as needed, one red line beneath the letter “C” suddenly emerged. The area beneath the letter “T” was left blank. I don’t have Covid if there is just one line. I do have Covid if there are two lines.
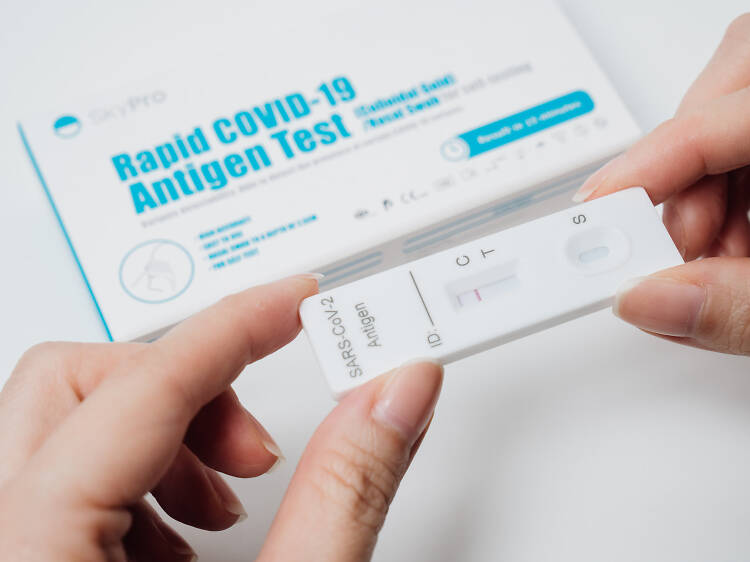
The red line under the letter C serves as confirmation that the exam was successful. The C line is really for “control,” although someone who didn’t read the instructions may think it was for Covid. Testing is indicated by the T line. The test is positive for Covid if you observe both a red “test” line and a red “control” line. However, if the C line is absent, there is a problem with the rapid antigen tests, and the findings are not accurate.
Timing Is Everything
The timing of any diagnostic examination is crucial. The test kits for use at home find viral proteins. Compared to PCR tests, which look for viral genetic material, they are less sensitive to detecting low amounts of the virus. As a result, home test kits won’t provide a positive result as quickly as a PCR test does when a person has an infection. This results in a frequent occurrence that we see with all diagnostic rapid antigen tests. Even though someone may already be unwell or infectious early on, the test results sometimes come back negative. That test result is referred to as a “false negative.” In this case, it is crucial to do a PCR test as a follow-up, particularly if you recently came into contact with someone who has known COVID or if you are experiencing symptoms of COVID. You can read about Coronavirus (COVID-19) pandemic by visiting https://www.health.gov.au/health-alerts/covid-19
The second problem is that home diagnostic kits lose their positive status more quickly than PCR tests do. As a result, a person who had Covid and tested themselves while already on the mend may likewise come back negative. Another instance of a false negative test result is this one. In this case, a follow-up PCR test is required if there is a genuine need to determine if someone received Covid. Remember that those with symptoms are often more likely to get good results from the fast home diagnostic tests, which allows for better scheduling.
The Value of Period Of Incubation
Every infectious disease has what is known as an incubation period, during which the microbe must develop in an animal or person before the disease may manifest itself or spread. A virus that enters your respiratory system multiplies rapidly within your body until its levels in your secretions are high enough for a test to pick it up. Sometimes the levels are high enough to infect someone else even if they are too low to be detected by the rapid antigen tests. Click here to read about Population testing for COVID-19.
This poses a significant problem for DIY test kits. Therefore, if you test yourself right after exposure, the result will be negative. Covid may take anywhere between 2 and 14 days to incubate, depending on the individual. This is why it is preferable to wait around five days following exposure before testing yourself. If not, you risk wasting a rapid antigen test kit. Just be careful about your interactions with others in the meantime, since you may initially be asymptomatic while Covid is developing inside of you but still be at risk of spreading it.
